Thank you for your interest in the Prescribing Safety Assessment (PSA).
The British Pharmacological Society and MSC Assessment are working together to deliver the Prescribing Safety Assessment (PSA) that allows all students to demonstrate their competencies in relation to the safe and effective use of medicines.
MSC Assessment and the British Pharmacological Society are working closely with all medical and foundation schools who have students due to sit the PSA over the coming months. If you have questions or concerns about your PSA sitting, please contact your school who will be able to provide you with the latest information.
If you are a medical or foundation school candidate expecting to take part in the forthcoming events instructions on how to register for the PSA online system would have been provided by your school. You must activate your account using the email link you have received and then login before you can access the PSA system. You are advised to do this as soon as possible in order to gain access to practice papers and information pages on the PSA.
Once you have successfully completed your account activation you will be able to view further materials to make you more familiar with the PSA assessment environment.
For general information about the assessment and its structure, click on the sections at the top of this page.
Prescribing is a fundamental part of the work of Foundation Year 1 doctors, who write and review many prescriptions each day. It is a complex task requiring knowledge of medicines and the diseases they are used to treat, careful judgment of risks and benefits of treatment, and attention to detail.
As well as offering the potential for improving health, it is an activity associated with potential hazards: a GMC-sponsored study found that 9% of hospital prescriptions contain errors ('An in depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education - EQUIP study'). It is also apparent in other research that this is the area of the Foundation Doctor role that new graduates find the most challenging (The state of medical education and practice in the UK report: 2014 and Be prepared: are new doctors safe to practice?). As a result, in Outcomes for graduates(originally published in Tomorrow's Doctors), the GMC defined prescribing competencies required of new medical school graduates.
The Prescribing Safety Assessment allows candidates to demonstrate their competencies in relation to the safe and effective use of medicines.
The Prescribing Safety Assessment (PSA) is a pass/fail assessment of the skills, judgment and supporting knowledge related to prescribing medicines in the NHS. The PSA assesses the prescribing skills of final-year medical students and is based on the competencies identified by the General Medical Council outlined in Outcomes for graduates (originally published in Tomorrow's Doctors). These competencies include writing new prescriptions, reviewing existing prescriptions, calculating drug doses, identifying and avoiding both adverse drug reactions and medication errors and amending prescribing to suit individual patient circumstances. The content of each item is relevant to the prescribing tasks expected of an F1 doctor, i.e. the questions refer to ailments and drugs that graduates are likely to be dealing with in year one of the Foundation Programme.
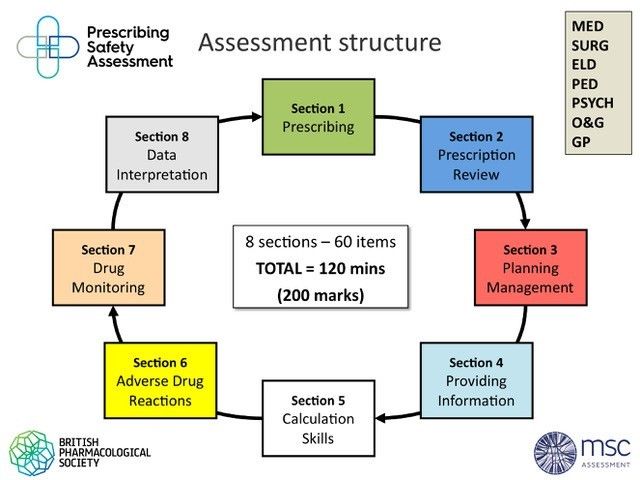
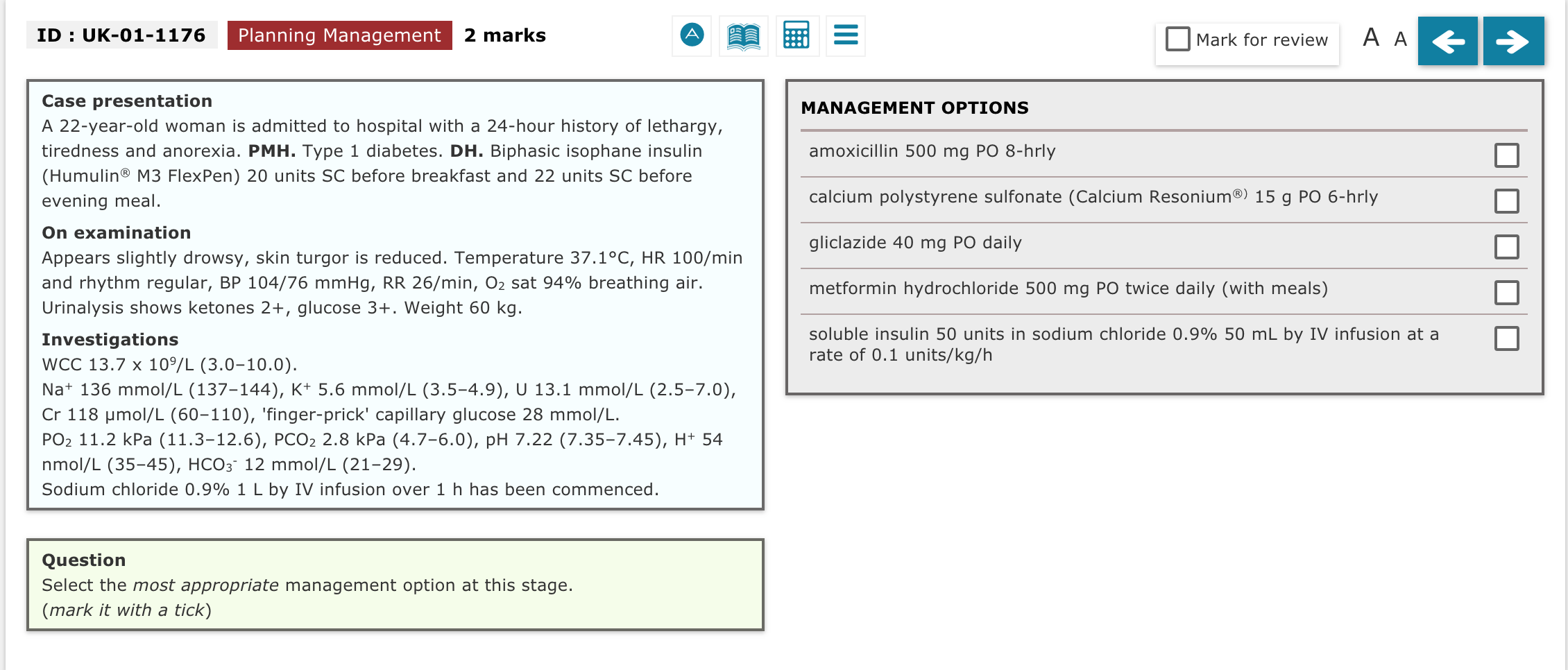
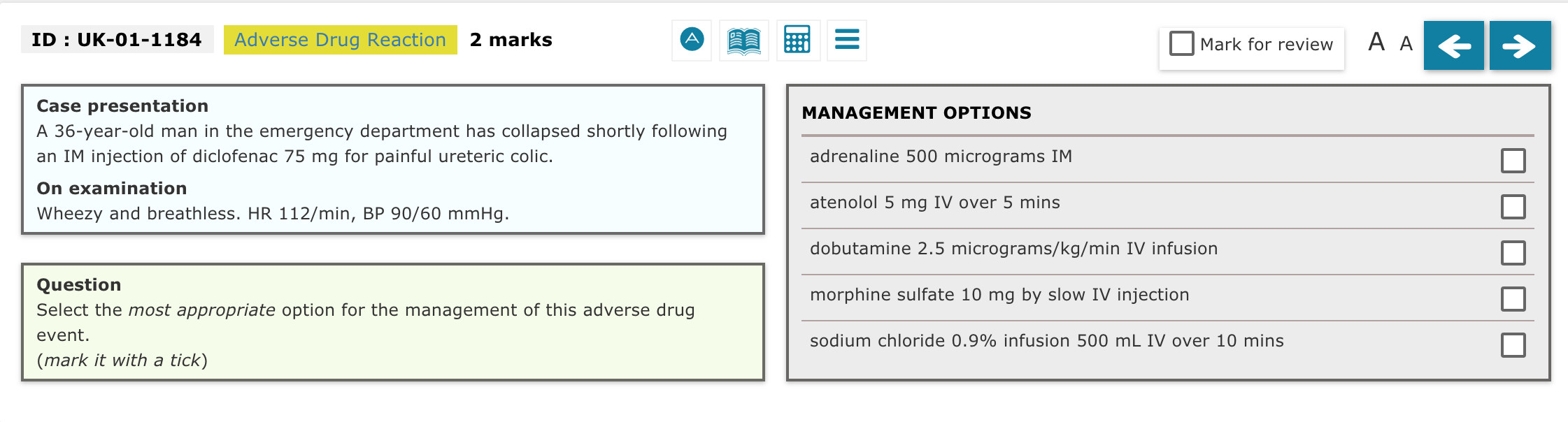
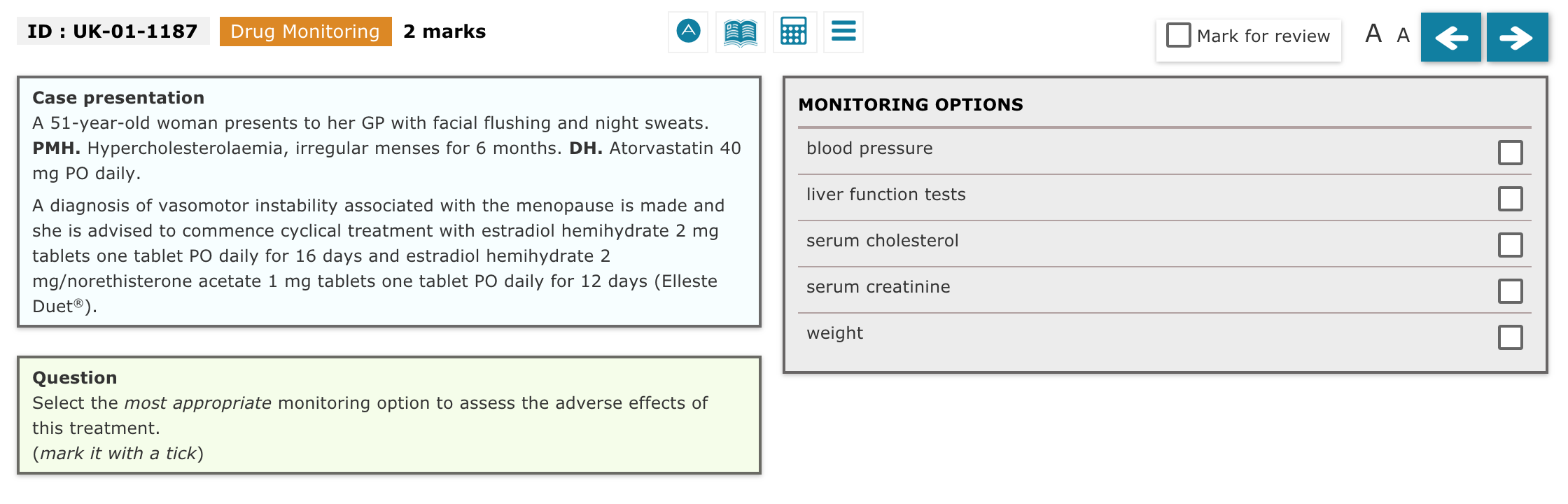
The Prescribing Safety Assessment Blueprint identifies eight different question types, each of which may be set in seven different domains of clinical activity:
| Question types | Domains |
|---|---|
| Prescribing | Medicine |
| Prescription Review | Surgery |
| Planning Management | Elderly Care |
| Communicating Information | Paediatrics |
| Calculation Skills | Psychiatry |
| Adverse Drug Reactions | Obstetrics & Gynaecology |
| Drug Monitoring | General Practice |
| Data Interpretation |
For a better idea of what assessment items look like please see the Example Question Items in the Resources section. Users who are registered by their school to take the final-year PSA gain access to interactive practice papers, which provide examples of what the assessment questions look like.
An update on our response to the PSA Independent Review
In August 2023, the Medical Schools Council (MSC) and British Pharmacological Society (BPS) welcomed the publishing of an independent review of the Prescribing Safety Assessment (PSA). The review, led by Professor Dame Jane Dacre, focused on how the assessment has impacted education and practice, and how it can be developed to strengthen prescribing knowledge and solidify its place as a valuable and worthwhile assessment.
While the recommendations in the report are welcomed, it is acknowledged that some of the ambitions will require further, long-term consideration. The current priority for medical schools remains ensuring that the Medical Licencing Assessment (MLA) is introduced effectively. To ensure both the MLA and PSA are complimentary, the MSC and BPS will explore how the PSA can be aligned in light of the introduction of the MLA. Following discussion with medical schools, it has been agreed that universities will remain responsible for choosing whether the assessment is used as a progression requirement or whether it is used as a non-progression exam. Nonetheless, passing the PSA will be mandatory for all newly qualified doctors as it remains an exit requirement for Foundation Year One.
There is consensus among medical schools that the PSA is an important measure of prescribing competence and is a useful and high-quality exam. This is also evidenced by a recent study by Magavern et al, which found that the PSA is a good test that measures how prepared someone is to prescribe. With its usefulness clear, we look forward to working together with medical schools and colleagues in the sector to use the PSA to ensure the doctors of tomorrow are safe and competent prescribers.
Prescribing is a fundamental part of the work of Foundation Year 1 doctors, who write and review many prescriptions each day. It is a complex task requiring knowledge of medicines and the diseases they are used to treat, careful judgement of risks and benefits of treatment, and attention to detail.
A GMC-sponsored study found that 9% of hospital prescriptions contain errors. It is also apparent in other research (see The state of medical education and practice in the UK report: 2014 and Be prepared: are new doctors safe to practise?) that this is the area of the Foundation doctor role that new graduates find the most challenging. In response, the General Medical Council (which regulates undergraduate medical education in the UK) has placed a much greater emphasis on the prescribing competencies expected of new graduate in Outcomes for graduates (originally published in Tomorrow's Doctors).
The aim is to assess the outcomes required of newly qualified doctors in Outcomes for graduates (originally published in Tomorrow's Doctors) as they relate to prescribing. The content of each question is relevant to the prescribing tasks expected of a Foundation Year 1 doctor as outlined in Tomorrow's Doctors 2009, so the questions refer to ailments and drugs that students are likely to be dealing with in Foundation Year 1. Students taking the test can refer to the content of the online British National Formulary at any point during the assessment. While the BNF is a recommended resource, it is important to understand it does not answer all questions on prescribing.
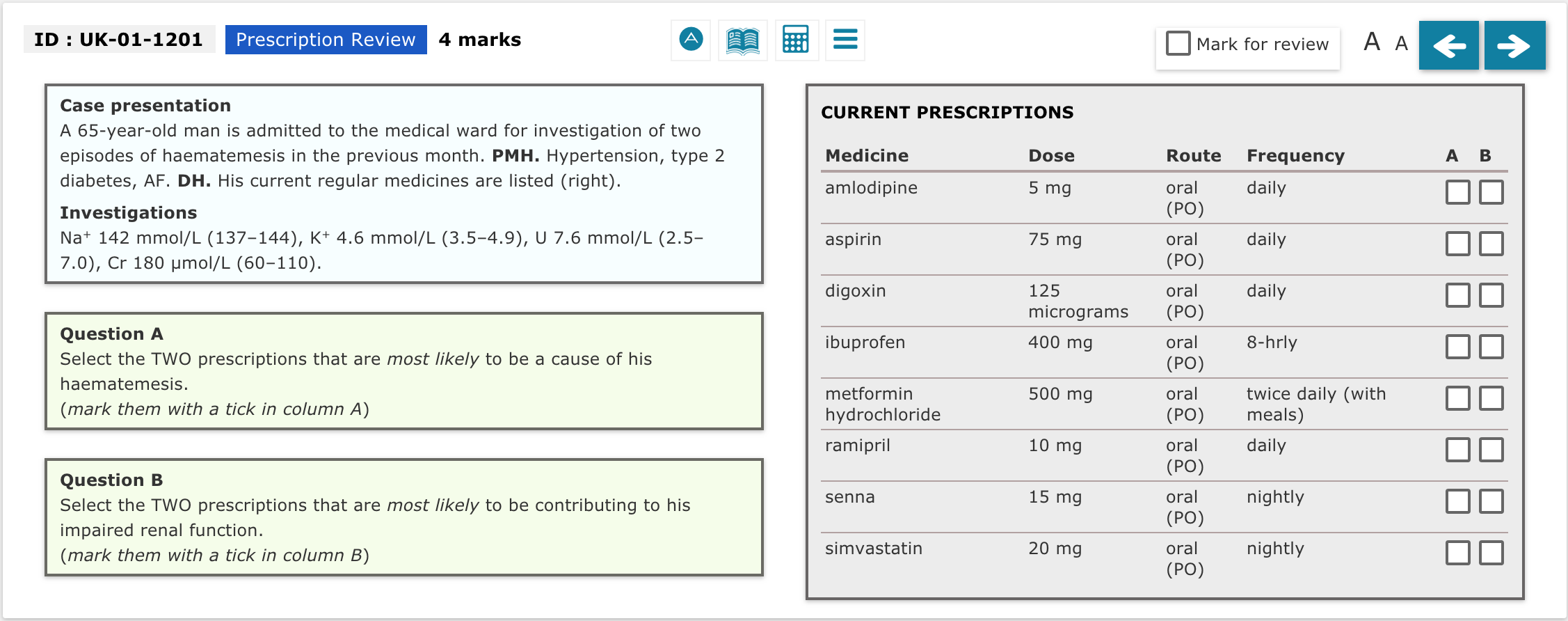
The assessment aims to test eight distinct prescribing sections across a range of clinical contexts: prescribing; prescription review; planning management; providing information about medicines; calculation skills; adverse drug reactions; drug monitoring; and data interpretation.
The MSC Assessment and British Pharmacological Society are leading the delivery of the PSA. They are supported by the Assessment Board, and a cross-sector Stakeholder Group. The Assessment Board to the PSA is responsible for overseeing the recruitment of experts to write and review assessment items and for developing quality assurance processes. The Stakeholder Group includes a student representative from the BMA, and enables key stakeholders, including medical students, to be involved in the development of the assessment and the associated policies and processes.
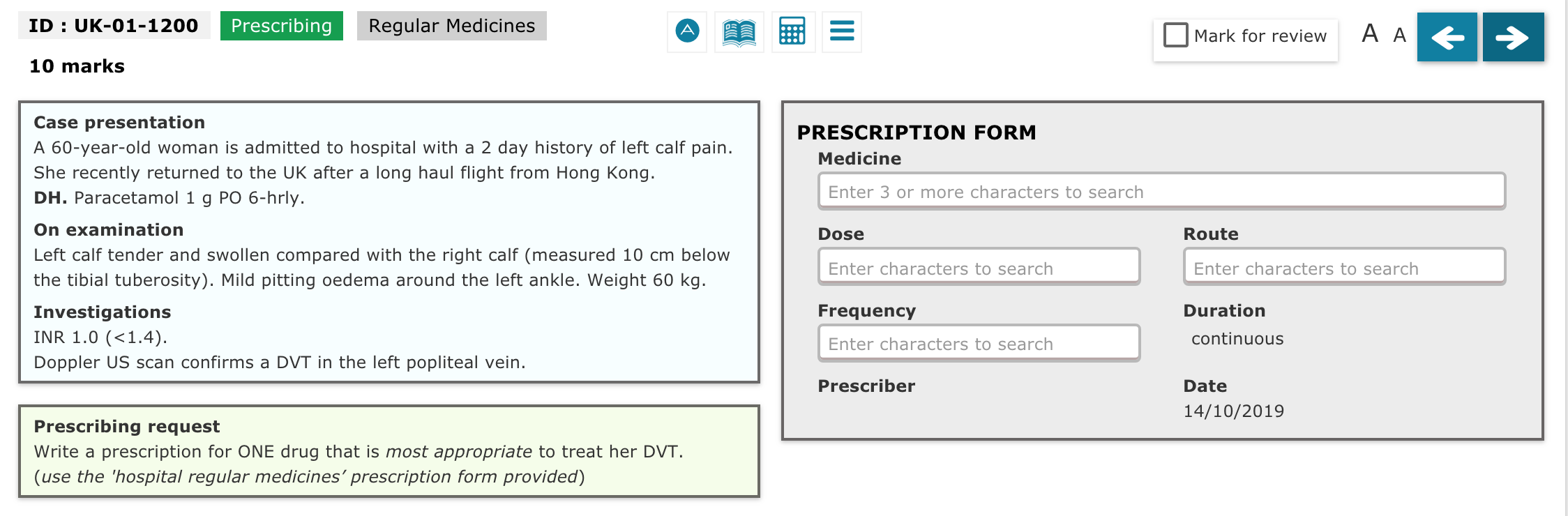
The questions that ask the candidate to fill a prescription chart carry 10 marks each: 5 for the drug choice and 5 for the choice of dose/route/frequency, making a total of 80 marks for this item style in a summative assessment. Please note that timing and signature fields are automatically populated by the system and no marks are awarded for them. For more information, please look at the PSA Blueprint document.
Please take a look at the forthcoming events.
In schools that use the PSA summatively, final-year students are required to take and pass the test in order to complete their medical degree. In other schools the assessment is formative and passing it is not a requirement for completing the medical degree. Students in these medical schools may still be required to take the assessment as a formative part of their medical education. Medical schools will communicate their requirements to their students.
By registering for the PSA, candidates agree that information about those who pass the assessment will be available to UK Foundation Schools. Those who have not passed the PSA in the two years prior to starting their F1 job will be required to pass the test before the end of their F1 year. A PSA sitting will be held by Foundation Schools for those F1 doctors who have not taken or not passed at the PSA at the start of F1. Doctors will be made aware of Foundation School/employer requirements for the PSA once doctors have been matched to individual programmes by their allocated Foundation School (April onwards).
F1 doctors applying for the UK Foundation Programme who have not taken or not passed the PSA prior to graduation will be expected to take the PSA with their foundation school. These candidates will be registered on the PSA Interface and notified by the foundation school when they can activate their accounts.
The pass mark for the PSA is set using the Modified Angoff method of standard setting. The exact pass mark cannot be published before the test as adjustments may be required to take into account differences in difficulty across papers and also any issues with items identified after the test has been sat. The passing standard of each question is defined by the Standard Setting Group, which is composed of undergraduate assessment experts from UK medical schools and representatives of the MSC Assessment Alliance
The prescribing items are marked using an automated system that compares the given answer with a mark scheme containing a number of correct answer(s) and suboptimal answers. The given answer must exactly match one of the answers in the mark scheme in all respects for credit to be given automatically.
Each answer is composed of several variables (drug description (including form and strength), dose, route & frequency) and therefore, a correct answer can be expressed in a variety of ways, depending on the product selected. Due to the breadth of possible answers, some credit-worthy variations may not be included in a given mark scheme and recognised by the auto-scoring system.
In the real assessment, the post-assessment review process considers every unrecognised answer and all credit-worthy answers are added to the mark scheme to enable marks to be credited.
This is one of the reasons why results release is delayed after each sitting; to make sure that no candidates are disadvantaged for providing answers that are not initially recognised but are credit-worthy.
Medical devices (including IUDs) are not included in the PSA drug bank, which is used to populate the drop-down menu of answers. Whilst they may be an appropriate treatment option in some PSA scenarios, the prescription-writing-skill (PWS) items are phrased to ask 'write a prescription for ONE drug . . . .' to which the optimal response would be a medicine, rather than a device or other therapeutic intervention. Knowledge of such devices may be tested in other item styles (e.g. planning management or providing information questions).
It should be noted that whilst the BNF contains lots of information that will be useful for the PSA, this information has to be taken within the context of the question. Furthermore, answering questions within the PSA requires more than a critique of information within the BNF; it requires an appraisal of the case history and use of student clinical experience gained in undergraduate training and related to commonly encountered prescribing scenarios at FY1 level. The PSA is not just a test of how well one knows the BNF but also of practical clinical experience.
Whilst the PSA assessment board will not comment on the content of PSA question papers, they can confirm that all questions are reviewed prior to each use to ensure they align with contemporary practice and guidelines. If guidance changes close to a sitting date, this is taken into account during the post-assessment review process, so that no candidates are disadvantaged by knowledge of recent changes in practice.
Your school will submit a list of candidates registered to take the PSA no later than four weeks before your test date. At this point, accounts will be created and the school will be informed when this is complete. The PSA Lead at your school will notify you when your account is ready to activate. If you have not received notification, please contact the PSA Lead at your school.
The PSA is an online assessment. The formats of the questions vary depending on what skill is being assessed; some ask the candidate to 'write' an appropriate prescription for a given problem, others ask the candidate to choose the most appropriate option from a list or to perform a calculation. Examples of what the items can look like can be seen on the Example Question Items page.
The PSA includes 60 items and is two hours in length. The length of the test may be reviewed in the future, in light of developments such as introduction of a national licensing exam and in respect of the stakeholders' views.
You will only be able to activate an account once your school has submitted a registration list for the PSA and received confirmation that the accounts have been created. This usually takes place four weeks in advance of the test date. In the first instance, please confirm with the PSA Lead at your school that they have registered you for the PSA.
If your account has been created and you are unable to activate it, or login once it is activated, please send a screenshot of the error message displayed to enquiries.psa@prescribe.ac.uk with the subject header "Login Problems".
The PSA Interface provides registered candidates with links to online BNF resources - BNF and BNFc on NICE website and well as BNF and BNFc on Medicines Complete. No paper copies are permitted.
The BNF is a recommended resource; however, candidates should understand that it does not answer all questions on prescribing.
In 2016, OpenAthens introduced a new authentication point as a security measure, which does not allow OpenAthens to work within iframes (i.e. the PSA practice papers). In order to use the BNF and BNF for children via Medicines Complete whilst completing the practice papers you will need to open a new tab on your browser and go directly to the Medicines Complete website.
Please note that access to the Medicines Complete BNF and BNF for children is enabled by IP address in the computer venues for the PSA. You do not need your OpenAthens login for the PSA and will be able to access the BNF directly within the test interface without being prompted for login details. It is advised that you also make yourself familiar with the NICE BNF and BNF for Children which is freely available and accessible during the PSA.
Candidates who are registered to take the assessment are granted access to three practice papers (two 30-item and one 60-item paper) within the assessment interface.
Candidates are strongly encouraged to complete all of the practice papers and review the individualised feedback as preparation for their exam attempt.
Medical school staff are granted access to the practice papers to support individual learners who are preparing for the PSA but should use different content in their own teaching materials.
Medical school candidates should contact their PSA Lead or assessment office. If you’re taking the PSA at a Foundation School, please request adjustments by contacting your Foundation School.
Please make the request at the earliest opportunity to allow time to accommodate it.
After each PSA sitting, a robust review of the paper performance is undertaken prior to results release. This includes a review of any unrecognised answers to prescribing questions, to make sure that any new answers are considered, and correct answers credited accordingly.
Following consultation with all UK medical schools, it has been agreed that results of the first PSA events of the year will be released within four weeks of the sitting (increased from three weeks) to allow more time for the initial review. The two-week window for the later exam sittings will not change. This revised timeline will apply from January 2025 onwards.
The PSA Lead at your institution will confirm when the results will be available to you on the PSA website as soon as the information is released.
All medical schools may decide to offer re-sits, especially if the PSA is taken as a summative test. Medical schools where the test is formative should also offer re-sits. Medical schools are responsible for providing further training and support in prescribing for those re-sitting, and they will inform their students of the local re-sit dates.
Current F1 doctors who did not pass the test at their Foundation School’s first sitting will need to undergo remediation and have two further opportunities to retake the test. F1 doctors who did not pass the test while at the medical school will be able to sit the test at their Foundation School.The PSA dates are listed here.
Candidates are advised to download a certificate with their performance soon after results become available on the PSA Interface in order to have a record for their future portfolio. Downloading the certificate may not be possible at a later date e.g. if the registered email address expires.
Candidates who took part in the PSA in the past and have not downloaded a certificate are advised to contact their medical school in order to receive another form of confirmation of their result.
Candidates are provided with feedback on their overall score in relation to the pass mark and on their score per each domain of the assessment. The local organising institution (medical or foundation school) notifies the candidates once these results become available on the PSA Interface. The details of individual questions and answers are not released as this may unduly focus attention on specific questions in a single paper, rather than on improving the generic skills and knowledge that are required for safe prescribing.
However, candidates are encouraged to attempt the practice papers which are available to registered candidates prior to their exam attempt. These papers provide detailed feedback about the optimal and suboptimal responses to each question, with guidance about the approach to take in answering the style of question. The papers can be attempted multiple times, and in most medical schools, a mock assessment is also available.
A PSA pass is considered valid for two years. If the PSA was passed more than two years before starting foundation training, it will need to be successfully retaken before completion of the F1 year.
Foundation doctors who have not passed the PSA before commencing the programme will be offered a support package and will be required to sit or re-sit the assessment. Further information is on the UKFPO website:https://foundationprogramme.nhs.uk/curriculum/prescribing-safety-assessment-psa/. Any queries should be directed to the allocated foundation school team.
Please note, if you pass the PSA at medical school and need to retake your final year, your medical school can decide whether they require you to retake the PSA or not. If you fail the repeat PSA, this will overwrite your previous pass and you will be required to re-sit. The PSA status is based on your most recent attempt.
It is advised you download and save in a safe place (eg cloud-based storage) your PSA pass certificate as accounts are disabled at the end of each academic year. If you no longer have access to your account and have lost your certificate you will need to contact your medical school who can confirm your PSA pass on university headed paper and can be used in place of the certificate.
If you are a clinical pharmacologist, pharmacist or other clinician with an understanding of the prescribing duties of an F1 doctor and are interested in writing assessment items for the PSA then please state your background and register your interest by emailing enquiries.psa@prescribe.ac.uk.
Resources for prospective and current item writers are available on Item Authors page and they can also view Example Question Items.
Access to the practice papers is limited to registered PSA candidates and tutors who are supporting individual learners to prepare for the PSA. Tutors are not permitted access to the mock paper, as this is designed as an 'unseen' paper.
The practice papers should only be accessed within the UKPSA interactive interface which is designed to allow multiple attempts and provides scores and adaptive feedback for each attempt. Therefore, the content must not be copied for use in other teaching materials. Candidates have unlimited access to the PSA questions, answers and feedback, which can be used in their own time.
Tutors may develop additional materials for use in their own teaching based on the example questions and formats which are available.
The PSA has limited resources and relies on the voluntary contribution of academic and clinical staff from around the UK who willingly give their time to create the content. Therefore, we request that these rules are adhered to, as they are intended to protect the experience of candidates accessing the practice papers.
Please contact the PSA team on admin@mscassessment.ac.uk to request access.
The PSA practice papers underwent significant review and restructuring in 2024.
The total number of practice questions is the same as previously, but some items have been replaced with newer content to reflect changes in clinical practice, new guidance and to better reflect the suite of current PSA items.
In response to feedback, we have restructured the content as two 30-item papers which are recommended for familiarisation purposes, and a 60-item paper, which is the same length as the PSA, to enable candidates who wish to run through a full paper in simulated examination conditions, the opportunity to do so.
We have provided indicative pass marks for all content.
We endeavour to make sure that all published content is up-to-date and reflects current prescribing practice and evidence.
We do not re-publish or circulate content that has been withdrawn.
More practice items are available to candidates who are registered by their medical school and activate their accounts.
If you are a clinical pharmacologist, pharmacist or other clinician with an understanding of the prescribing duties of an F1 doctor and are interested in writing assessment items for the PSA then please state your background and register your interest by emailing enquiries.psa@prescribe.ac.uk. Feel free to browse through the item writing templates and style guides below in order to gain a sense of what item writing involves.
Resources for authorsPlease use the PSA Item Writing Manual to guide you when writing new items.
Workshop presentationsProject Team presentations from the September 2015 PSA Training Workshops can be found and downloaded below.
The Prescribing Safety Assessment (PSA) is delivered through an equal partnership between two organisations: the British Pharmacological Society and MSC Assessment.
The assessment is developed through a cycle of the following four workstreams.
- The PSA Executive Board - responsible of the strategic direction of the PSA
- The PSA Assessment Board – responsible for item and test development
- The PSA Standard Setting Group – responsible for the standards of the assessment
- The PSA Stakeholder Group - enables effective engagement and feedback with key representatives including medical students and the General Medical Council
Information about the membership of these groups can be found using the links above.
The PSA Assessment Board takes responsibility for overseeing the quality assurance process, which ensures that PSA question items entered into the item bank are fit for the intended purpose and assess the prescribing-related competencies described in the blueprint. The Board selects question items from the item bank to create PSA assessments, supervises the work of the standard setting group and reviews the performance of individual items during summative assessments. The initial Assessment Board was convened during 2012.
The PSA Standard Setting Group determines the passing standard for each assessment developed by the Assessment Board.
If you experience any difficulties, please send your enquiry in a detailed email outlining the problem to enquiries.psa@prescribe.ac.uk.
To contact the PSA Project Team: enquiries.psa@prescribe.ac.uk
To contact the British Pharmacological Society: www.bps.ac.uk
To contact the MSC Assessment: www.medschools.ac.uk